Transcript of Jan. 28, 2004 videotaped conversation with ALS specialist, who confirmed brainhell's ALS diagnosis.
So, You're Going To Die!
Doctor1: Unaccustomed as I am to doing this on camera, let's talk a little bit about, first of all, where we are. So, what have you been told to far?
Brainhell: What I've been told by Dr. XXXXXXXXX is that, based on what he's seen, he believes I have ALS, but I need to be evaluated by you guys.
D: So, he told you he thought it was likely to be ALS?
B: Yeah.
D: Did he discuss with you what that is?
B: Yeah, I know what amyotrophic lateral sclerosis is, also known as Lou Gehrig's disease, a progressive incurable neuromuscular degeneration, typically... typically kills most people within four years of diagnosis, but there are some exceptions.
D: Actually a lot of exceptions.
B: OK.
D: OK, so do you want me to shoot completely straight with you?
B: Go right ahead. Yes.
D: Tell you everything--
B: Yes.
D: ...that I'm thinking?
B: Yes. Yes. The more the better, yeah.
D: Even if the news isn't entirely good?
B: That's fine. Yeah.
D: OK. It's not entirely good.
B: I cope very well.
D: OK.
B: Yeah.
D: So I first of all have to say that this really does look like ALS.
B: OK.
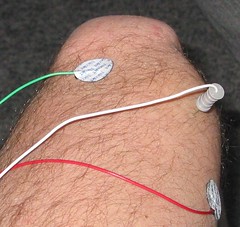
D: Uh, I come reluctantly to that diagnosis because one never likes to make it. And yet the way this has come on you, this kind of gradual onset of the difficulty with your hand and your foot, and then looking at the MRI, and looking at your reflexes and the twitching, and seeing the results of the EMG, all of this looks really very like ALS.
B: OK.
D: So I have to say I'm fairly sure that that's what it is.
B: Yeah.
D: I would recommend a couple of blood tests that we do that are kind of specialized, in the spirit of turning over every stone, and making sure that there has nothing been missed. Because we do not have a test that's absolutely conclusive that would tell us 100 percent for sure that this is ALS. So what we have to do is really be sure that we haven't missed anything that could look like ALS. And by doing the EMG studies and the MRI studies, we're getting upwards of 95, 98 percent confidence level.
B: OK.
D: And a few additional blood tests to just be sure, and sometimes we get something out of the blood studies, so I want to keep a little hope that we might uncover something that we could actually do something about. So, do you have any questions about what I've said so far?
B: What would the blood studies be looking for?
D: Um, mostly looking at your metabolism, to see if there's any inflammation in your system, any abnormal protein that might be irritating your nerves.
B: OK
D: Anything with the metabolism, the way your body is handling vitamins and calcium and thyroid and some of the things that really sometimes can effect the motor nerves.
B: OK.
D: So, it's a simple thing to do. Kind of in the category of being a long shot.
B: Yeah.
D: But still worthwhile because occasionally we find something.
B: Right.
D: OK?
B: OK.
D: So, if those tests are all normal, then that really will give us a high confidence of the diagnosis. And so what I'd like to do is chat with you a little bit, on the assumption that the test are going to be normal, and OK let's say 'What if?' What if the worst case scenario is true? What if it really is ALS, what does that mean? And the first thing to say is that really everybody is different, with ALS. So, I've seen some people who, within nine months, are dead, from this disease. It's very rare, fortunately. And then other people who have either fully recovered from it, or who have been successfully managing the disease for more than 20, 25 years. And then everything in between.
B: Two questions. What information source can you refer me to that will describe, you know, the statistical breakdown etc. etc. of the variance that you just talked about? And the other thing is, would you say that the EMG result was pretty classical ALS?
D: I believe.
B: OK. What book, or what should I read in order to educate myself about variance in ALS?
D: Well, um, most of the books that I could tell you about are not written for the lay person, but you're very bright and it might be that you could deal very well with these.
B: I'll give it a try.
D: Yeah. [Speaking to second doctor] And so, we can give him, afterwards, if you're reminding me, we can give him a couple of titles.
B: [Speaking to second doctor] And I have your email address and I might ask.
D: So, to summarize all that though, is, what we find is that ALS is not just one disease.
B: OK.
D: We suspect that there are different types of ALS.
B: Yeah.
D: The type that you have, in a preliminary fashion...
B: I understand.
D: I'm just trying to hedge my bets a little bit...
B: Yeah.
D: But there are several things about your situation, and this relates to the question you just asked me, about how do you gauge severity, and the future, and outlook, and what we call 'prognosis.'
B: Right.
D: And, how old are you?
B: 40.
D: So, being young is a very positive prognostic factor. That's probably because we're all losing cells as we get older, and at the age of 40 you have a huge safety factor in your nerve cell population. So age is especially positive. Having mostly what we call upper motor neuron abnormality as opposed to a lower motor neuron abnormality...
B: Uh huh.
D: Do you know what that is?
B: I understand the distinction, yeah.
D: OK, so the fact that you have mostly the slowing and the shaking...
B: That's upper.
D: That's upper motor neuron, rather than thinning and weakening, which is lower.
B: Uh huh.
D: People who have primarily upper motor neuron dysfunction have generally a much better outlook. Generally a slower form of the disease. Generally do much better.
B: OK.
D: So the age and the predominance of the upper motor are very, very positive. And even though I hear you about your swallowing, everything that we see about your speech and swallowing muscles seem to be normal.
B: OK.
D: And everything that we see about your breathing muscles seems to be normal.
B: OK.
D: So when the, what we call the bulbar muscles, which are these muscles in here for speech and swallowing, the respiratory, the speech and swallowing muscles appear to us to be normal. These are two very positive prognostic factors. Both of those things. Either one of those being abnormal is serious. Both of them being normal, at the time of diagnosis, is very positive.
B: OK.
D: So, being a man is not quite as good as being a woman.
B: OK.
D: But it's not a big difference, but women actually seem to fair a little bit better than men. But that's a subtle difference. So you've got really most of the very positive prognostic factors going for you. And I have had people who have predominantly the upper motor neuron type, and who are predominantly young, who have normal breathing muscles and normal, apparent -- to us -- normal swallowing and speaking muscles, who have a very slow form of the disease. A much more benign type of ALS. I could be wrong. I love it when I'm wrong. But that's how it looks to me.
B: OK.
D: So having said the really serious, bad news that I do think this is ALS, I do want to say to you that it looks to me as though you may have a more slowly-progressive form than the great majority of people that we see.
B: Two questions.
D: Sure.
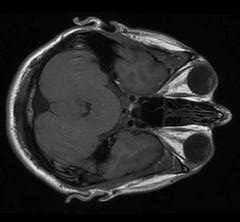
B: Um, first question is, how do I establish a metric and then sort of test and gauge myself in order to make a projection? And second thing is, what did you think of the brightness of the FLAIR signal in the MRI?
D: Well, the MRI is abnormal. And it does indicate to us that it's more confirming information. It does support the diagnosis of ALS. The pattern of that FLAIR signal is really very typical of ALS. And now that we're starting to become more experienced with the FLAIR images in MRI, we're finding that that can be very helpful in making a diagnosis or at least in supporting it.
B: OK.
D: It doesn't tell us anything good or bad, it just tends to say that it's really very typical of what we see in ALS.
B: OK. What about gauging, measuring my own progress?
D: Well, the things that are really important are of course your functionality, which you will be able to see very well. The things that we focus on are the breathing measurement, because generally speaking that is the most important single measurement that we make.
B: The 94, I scored a 94, is that cubic centimeters?
D: No.
Doctor2: It's a percentage of the average normal value.
B: OK.
D2: That's within the normal range.
B: It's a percentage.
D: It's percent of predicted.
B: Like the typical population at my age or whatever.
D2: Your height...
B: Would be 100 percent, sorry, would be 100. And I was 94.
D2: Right.
D: You're at the 94th percentile...
B: Percentile.
D: ...of people for your age...
B: Yes.
D: ...weight, height, and gender.
B: So when...
D: We have a huge data bank and when anyone is over the 85th percentile, of the huge data bank...
B: Yes.
D: Your familiar with the [Gestures]...
B: The bell-curve, yeah...
D: ...the bell-shaped curve, you're what we would consider normal.
B: OK.
D: So that measurement, as we're very experienced with it, and do that each time we see people with ALS, allows us to kind of track how things are going.
B: 94th percentile -- sorry to interrupt -- 94th percentile actually, to me seems very good. I mean, like, when I took--
D2: It's not exactly a percentile. It's a percentage. Of a predicted value.
B: OK.
D2: Which would be a 100 percent, and you're 94 percent.
B: All right. Sorry, I interrupted you.
D: So, are we OK then so far, with what we have?
B: Yeah, I just--
D: Most people do have a periodic visit to a center like this, where we make measurements, and kind of give feedback about how things are going. The average person comes here about every three months. This may or may not be appropriate for you, but we can tell you what our resources are and you can decide whether you want to use us any in the future. The big things that we do here are, first of all, we're heavily involved in research, and we're testing new compounds, and I'll tell you about that if you're interested.
B: The availability of studies, clinical trials?
D: Yes, yes, right. And then the second thing is that, um, we have a comprehensive team of experts in every conceivable aspect of this condition. Hand functions, speech functions, swallowing functions, nutrition, exercise, mobility, on and on. Every aspect of the disease is represented in our team of experts for rehabilitation and for giving therapies and things that would help you.
B: Yeah.
D: So what you might consider is coming here one time to see what the team could offer you in a one-stop shopping sort of thing, and that would probably be something that you would want to allow a half day for, and sometime in the next month or two, depending on your schedule. And you'd get a good feel for what we have available. And most people find it extremely helpful. So, we would -- and, and the average person comes here about every three months for that kind of comprehensive care and evaluation and indication of how things are going and what can be done.
B: Yeah.
D: So, and then, on the research side we're testing some new compounds that we think are very promising, very exciting. And we'd be happy to give you some information about that, for you to decide whether you might be interested.
B: Oh, yeah.
Wife: I think one concern that we discussed is, what's the chance, of our testing them, that he might wind up getting a placebo rather than the actual substance?
D: Right. So everybody has a chance of getting a placebo, and some people decide that if there's a chance of getting a placebo, they're really not interested, and we totally understand that because being in research is optional. Other people say: What do I have to lose? If I do nothing, I have no chance of benefiting myself or helping other people or really fighting to stamp out the disease. So, to some extent there is an altruistic motive, but to some extent there is a motive of possibly getting benefit. And then the third thing that happens with the people who are in the trials are first of all, there's a tremendous sense of optimism in people who are in trials compared to those who aren't, and people who are in trials come here regularly and actually get better care, because they not only have a finger on the pulse of what's happening, but they get a lot of attention when they're coming here. There's no cost for any of that, it's all, all free.
B: And typically you're only in one trial at a time?
D: Yes, you do have to kind of 'pays your money and takes your chances.'
B: You can go sequentially, right?
D: Well, you can do one and then do another.
B: OK.
W: So currently for the treatment of ALS or trying to slow the progression there's not like a cocktail of drugs the way there is for HIV?
D: That's where we're moving. We want to develop a cocktail. At the moment we have one drug, riluzole. And, you're not taking it, right?
B: No I am not.
D: So we'll discuss that next.
B: OK.
D: But where we're going is to get multiple drugs. We have this on drug that slows down the disease course. It's very safe. And what we want is to develop a cocktail of drugs like AIDS and leukemia. We do know that high doses of vitamin E, added on to the riluzole, add or enhance its effect a little bit. So we do recommend 2000 vitamin E a day with some lipid or fat or milk or something in the tummy to help facilitate the absorption of it.
B: [Fumbles for pen]
D: You've got it on tape.
B: Yeah! I got it on tape. Yeah.
D: [Laughing] You've go everything here, you don't have to write down a single thing!
B: No, I...
D: And where we're after is another drug or two to add to that cocktail. So we have the beginnings of a cocktail. So this drug riluzole suppresses too much glutamate, which appears to be an issue.
B: Glutamate.
D: The buildup of glutamate in motor areas in ALS that appears to cause some of the mischief. And riluzole blocks that, and it does slow down the disease process. And even though the literature on riluzole says it gives you an extra couple of months, that was on the results of people tested who were much farther along the disease course than you. And what we're now seeing, in Ireland and in Britain and in other registries where people are starting the drug earlier, that there's a substantial benefit from the drug. It's very safe, but it is very expensive. And so, um, you would have to decide about the cost factor because, Kaiser used to pay for it, and now my understanding is that they may not longer be covering the drug.
B: Just FYI, I'm on Blue Cross PPO.
D: [Thumbs-up sign].
B: Yeah. [Thumbs-up sign]
D: Good. Sounds good.
B: Um, but...
D: So do you have questions about the drug.
B: Um, tell me about the...
D: It's a pill.
B: ...the cost factor.
D: You take it twice a day. Well, if you're just buying it, it's 800 a month.
B: Flat. Eight hundred a month?
D: Something like that, you know, give or take--
B: But then I have some, I do have coverage, so they'll pick up the, hopefully part of it. But I just want to respond and says, yes, you guys are the experts and I do want to avail myself and be involved here and probably be in some of the clinical trials...
D: Great.
B: Um, riluzole sounds very interesting. I was supposed to ask you about that. Um, there are -- you mentioned the vitamin E. There are various question that I have. You probably have literature that can answer them, so I really don't need to take up your time about what should I do now, right? Um, do you think it is a bad idea -- I'm taking 2.1 grams of creatine, uh, have been since the 18th of January. Is that a bad idea?
D: No.
B: OK.
D: For now I wouldn't change that.
B: OK.
D: Uh, and for now I would only do two new things.
B: OK.
D: Add 2000 of vitamin E, and then, riluzole.
B: OK.
D: And not try, not do multiple things at the same time.
B: Right.
D: So, and then, when you get stabilized on those, on the vitamin E and riluzole, and the creatine, then we can talk about whether other things might be useful.
B: OK. Can I get a prescription for riluzole? [points to second doctor]. You're -- That's what you're. [Laughs] OK. And can I fill it somewhere around here?
D: Well, here's the deal...
B: Or, or the...
D: Yes, and yes. But just be aware that for you to get riluzole from the Kaiser system, that would have to be prescribed by a Kaiser neurologist.
B: I'm on the PPO. Blue Cross, not Kaiser.
D: OK.
B: Um. Can you briefly, very briefly, tell me what, now what is creatine?
D: Well creatine is a supplement that actually has a beneficial impact on the mitochondria. The mitochondria is the energy factory of the cells.
B: Right.
D: So the good news is that in a mouse model of ALS, creatine prolongs survival and seems to really be of substantial benefit. The bad news is that two studies that have been done so far in patients with ALS, using creatine, have so far shown no benefit.
B: Right.
D: There is a third study under way though, looking at it in a new way [gestures], and so, that's what it does.
B: OK. Is it ... It is not a hormone, right?
D: No.
B: DHEA if I understand it is a...
D: That's a hormone.
B: ...hormone precursor? Or is it a hormone?
D: Well, it's a hormone and it's a hormone precursor.
B: OK.
B: Creatine is just ... what ... is it an enzyme or a protein? I don't know?
D: Um, I don't know how to classify it.
B: OK.
D: [To second doctor] Do you know how to classify it?
D2: It's a protein.
W: Amino acid?
B: Apparently they've known about it since, like 1859.
D: Oh, yeah.
B: OK. [To wife, running camera] You have a list of questions.
W: Well, already some of them have been answered, but I did want to ask about the role of exercise. I mean, [B] has been trying to run or lift weights and do yoga, whatever. He's done something almost every day, sort of on the theory of you either lose it, uh, use it or lose it. And so, I'm wondering if that's something... Maybe it's something a physical therapist would address more.
D: Well, if you come to our clinic, our physical therapist will address that in great detail. But what I would say to you is that uh, we are bullish about exercise. And we feel that it's helpful, and desirable. The only caveat there is, we don't like to see people overdo. So, when you feel tired, stop.
B: OK.
D: And if you have pain the next day, you overdid. And, short of that, no problem.
B: OK.
W: OK, well, then I wondered about other factors, and would they have any effect on the, diagnosis. For instance like having a high cholesterol, does that have anything to do--
D: No.
W: Would it effect the disease at all?
D: No.
W: OK. Let's see. I was happy to hear that he falls into the category of having a slower rate, or...
D: Yeah.
W: There are several factors that point towards that.
D: We interpret that as being very positive.
W: Um.
B: That is very positive, yeah.
W: Yeah, and we have two, because we have two small children, and the thing that came to my mind when we first heard the diagnosis was that, you know, if he was you know, needing to breathe with a respirator any time soon, we're going to be bringing home all kinds of germs from school, and how do you handle that?
D: OK. If and when we come to that, which is way down the road, don't worry, we'll all deal with that.
W: OK, and then ah, yeah I guess you've answered most of these, most of my questions. I guess the last thing was that I looked at one website that suggested that as soon as you've gotten the diagnosis, the whole family should go into counseling, but with a four-year-old and a one-year-old, it doesn't seem the right thing to do, so what would you recommend?
D: Well first of all, when we say the whole family, we're really talking about the two of you. Uh, little kiddos, uh, you know, wouldn't really be able to comprehend this and we don't recommend making any big deal out of it for little kids. You know, if they were a little older, or if you were having more trouble, they would need to have some explanation, but it should be something very simple. 'Dad's having trouble with his leg, it's nothing to worry about.'
B: Yeah. Right.
D: That type of thing. For older kids it's a different story, but for little kids that's what we recommend.
B: Yeah, I thought so.
D: So, the other things that we know that a correlated with longevity with this disease...
B: Yes.
D: ...are not giving up, or giving in, having an upbeat attitude, having a strong support system, and ...
D2: We're three for three.
B: Yeah! [Laughter].
D: And the other one is, uh, not getting depressed. Or, if one does get depressed, having some treatment for depression. Many people get depressed with this condition, and often it's temporary. Have you been depressed since this has come up?
B: No, I've been, at times, we've been angry or just very distraught.
D: Yes.
B: But that usually lasts -- I feel a little that way now, just thinking about it.
D: Yes.
B: But that lasts a couple of hours. But I'm really a very positive person.
D: Yes.
B: I'm not trying to, I don't force. When I was a boy, between like ages 9 and 19, OK, I was depressed. So I know what that feels like. I'm not depressed. And I ...I don't. I don't think I'm at risk but I'll watch out for it.
D: So, do that. Only in the sense that, hey, we can give you medications for that that would really be helpful.
B: Sure.
D: [To wife] And you too need to look for that in yourself.
W: Uh huh.
D: As well as in him. Because we use antidepressants here like water. And often we need them only for a short time. And many people do need them. And it just speeds the adjustment tremendously for people who do get down.
B: OK.
D: So just keep an eye peeled. It doesn't happen to everybody. But if it does happen, just be aware and support each other and know that treatment really makes a lot of sense, with some medication.
B: I know you have tremendous resources here. How do I get on that train? Like, I could go home and get in ... get distracted and... What I'm saying is, how do I involved?
D: Plugged in?
B Plugged in. Sorry, that's--
D: Well we have two team members who are here who can plug you in. They're going to come in and talk to you.
B: Good. Excellent.
D: You OK, for the time?
B: Yeah. That's perfect.
D: OK.
B: Yeah.
D: Any other questions right now?
W: I was just wondering, are there alt-- I mean, you said the riluzole is the drug that's most, got the most, ah, experience behind it and so then that's what you recommend to start with. Is there--
D: It's the only FDA-approved drug...
W: I see.
D: ...to slow down the disease. And then vitamin E we say because it seems to enhance the riluzole effect.
W: So, as far as starting on something that would perhaps have a positive effect, that would be the only alternative right now at this point.
D: Right. And then if one decides about the clinical trails, to participate in a trial, that has the real potential of helping too.
B: Yeah, I'm excited about that.
D: Good.
B: I have two questions for you. One may make you laugh, ridiculous. I used to be a knuckle cracker. All the time. And I forced myself to stop cracking my knuckles probably, maybe seven years ago. Any even remote possibility that this --
D: No.
B: OK. Next question.
D: Let me just say, everybody wants to know what brought this on. Everybody.
B: And we don't know that the cause is.
D: You got it.
B: Yeah.
D: You got it.
B: OK.
D: It's nothing you did wrong.
B: All right.
D: For sure. It's nothing you did wrong.
B: OK. Next, and this is the harder question: Can you, please -- and I know this is difficult. Can you give me the rosy scenario in terms of number of years and how functional, and when I might eventually die of this, and give me the dark scenario.
D: Well the dark is that you could die within a year. Highly unlikely, given the things that I've already told you about. The rosy scenario ... the rosiest scenario...
B: Yeah.
D: ...is that this might turn around and even go away. I've seen that.
B: How often -- how -- what percentage of people does that happen to?
D: Small.
B: Very small.
D: Yes.
B: OK. Let's assume it doesn't go away.
D: Then the next most rosy scenario is that this goes very slowly, and a year from now we're sitting looking at each other and the differences are very modest.
B: OK.
D: Little more trouble with the hand, little more trouble with the leg. A year later we're getting together, and it's still only in the left arm and leg and we're still looking at a only a little bit of worsening. And I have seen that.
B: OK.
D: So, that's -- worsening over time -- but very, very slowly. So that would be second-best rosy scenario.
B: Gimme a number on that one.
W: Percentage.
B: I know it's hard.
D: What percent?
B: No, when do I die, basically, under the, the sec--
D: Well, the first one, obviously you would not have shortened life.
B: Right. Right.
D: Complete recovery.
B: The second...
D: The second one, you might have a normal life span.
B: OK. That's what I intend.
D: Yes. Absolutely. And you know the one patient that I can think of very clearly who did fully recover from this is now 96 years old.
B: Wow.
W: Wow.
D: Absolutely full of spit and vinegar and refused...
B: Yeah.
D: ...to let this get her down.
B: Yeah.
D: And, I swear, it was the attitude.
W: How old was she when she was diagnosed?
D: 72.
W: Yeah.
D: I've been seeing her for 24 years.
B: Amazing.
B: Can I ask you both a question?
D: And then I have to go.
B: OK. Um, my right side, um ... how impaired does it seem? I mean, I notice, I can do this [tapping forefinger on thumb rapidly] but I my wife, and you, can do it faster.
D2: Yeah.
D: And so I would say, minimal.
B: OK.
D: Minimal.
B: All right. All right. Well, I thank you. [Handshake].
D: So we're going to have a couple of other people come in and talk with you about what services we have, and the clinic, and so forth.
B: OK.
D: And then, um, we're here for you.
B: All right.
D: So whatever you decide... I know you're going to be checking back in with Dr. XXXXXXXXX. Many people use our services along with their local neurologist, and find that there's different benefits for both. Some people just go back to their neurologist. That's fine. Other people just come here. And any admixture, whatever works for you, we will work with.
B: OK. All right.
W: What would you say that the local neurologist could offer that you could not, or that he could offer more easily?
D: Proximity.
W: Yeah.
B: Like, 'Hey, look at this!'
D: You got it.
B: OK.
W: Thank you.
D: Thanks.
D2: I have a few things for you.
B: OK.
D2: [To camera] And... Cut!
W: OK.
[next tape segment]
B: Big Whoop!
So, You're Going To Die!
Doctor1: Unaccustomed as I am to doing this on camera, let's talk a little bit about, first of all, where we are. So, what have you been told to far?
Brainhell: What I've been told by Dr. XXXXXXXXX is that, based on what he's seen, he believes I have ALS, but I need to be evaluated by you guys.
D: So, he told you he thought it was likely to be ALS?
B: Yeah.
D: Did he discuss with you what that is?
B: Yeah, I know what amyotrophic lateral sclerosis is, also known as Lou Gehrig's disease, a progressive incurable neuromuscular degeneration, typically... typically kills most people within four years of diagnosis, but there are some exceptions.
D: Actually a lot of exceptions.
B: OK.
D: OK, so do you want me to shoot completely straight with you?
B: Go right ahead. Yes.
D: Tell you everything--
B: Yes.
D: ...that I'm thinking?
B: Yes. Yes. The more the better, yeah.
D: Even if the news isn't entirely good?
B: That's fine. Yeah.
D: OK. It's not entirely good.
B: I cope very well.
D: OK.
B: Yeah.
D: So I first of all have to say that this really does look like ALS.
B: OK.
D: Uh, I come reluctantly to that diagnosis because one never likes to make it. And yet the way this has come on you, this kind of gradual onset of the difficulty with your hand and your foot, and then looking at the MRI, and looking at your reflexes and the twitching, and seeing the results of the EMG, all of this looks really very like ALS.
B: OK.
D: So I have to say I'm fairly sure that that's what it is.
B: Yeah.
D: I would recommend a couple of blood tests that we do that are kind of specialized, in the spirit of turning over every stone, and making sure that there has nothing been missed. Because we do not have a test that's absolutely conclusive that would tell us 100 percent for sure that this is ALS. So what we have to do is really be sure that we haven't missed anything that could look like ALS. And by doing the EMG studies and the MRI studies, we're getting upwards of 95, 98 percent confidence level.
B: OK.
D: And a few additional blood tests to just be sure, and sometimes we get something out of the blood studies, so I want to keep a little hope that we might uncover something that we could actually do something about. So, do you have any questions about what I've said so far?
B: What would the blood studies be looking for?
D: Um, mostly looking at your metabolism, to see if there's any inflammation in your system, any abnormal protein that might be irritating your nerves.
B: OK
D: Anything with the metabolism, the way your body is handling vitamins and calcium and thyroid and some of the things that really sometimes can effect the motor nerves.
B: OK.
D: So, it's a simple thing to do. Kind of in the category of being a long shot.
B: Yeah.
D: But still worthwhile because occasionally we find something.
B: Right.
D: OK?
B: OK.
D: So, if those tests are all normal, then that really will give us a high confidence of the diagnosis. And so what I'd like to do is chat with you a little bit, on the assumption that the test are going to be normal, and OK let's say 'What if?' What if the worst case scenario is true? What if it really is ALS, what does that mean? And the first thing to say is that really everybody is different, with ALS. So, I've seen some people who, within nine months, are dead, from this disease. It's very rare, fortunately. And then other people who have either fully recovered from it, or who have been successfully managing the disease for more than 20, 25 years. And then everything in between.
B: Two questions. What information source can you refer me to that will describe, you know, the statistical breakdown etc. etc. of the variance that you just talked about? And the other thing is, would you say that the EMG result was pretty classical ALS?
D: I believe.
B: OK. What book, or what should I read in order to educate myself about variance in ALS?
D: Well, um, most of the books that I could tell you about are not written for the lay person, but you're very bright and it might be that you could deal very well with these.
B: I'll give it a try.
D: Yeah. [Speaking to second doctor] And so, we can give him, afterwards, if you're reminding me, we can give him a couple of titles.
B: [Speaking to second doctor] And I have your email address and I might ask.
D: So, to summarize all that though, is, what we find is that ALS is not just one disease.
B: OK.
D: We suspect that there are different types of ALS.
B: Yeah.
D: The type that you have, in a preliminary fashion...
B: I understand.
D: I'm just trying to hedge my bets a little bit...
B: Yeah.
D: But there are several things about your situation, and this relates to the question you just asked me, about how do you gauge severity, and the future, and outlook, and what we call 'prognosis.'
B: Right.
D: And, how old are you?
B: 40.
D: So, being young is a very positive prognostic factor. That's probably because we're all losing cells as we get older, and at the age of 40 you have a huge safety factor in your nerve cell population. So age is especially positive. Having mostly what we call upper motor neuron abnormality as opposed to a lower motor neuron abnormality...
B: Uh huh.
D: Do you know what that is?
B: I understand the distinction, yeah.
D: OK, so the fact that you have mostly the slowing and the shaking...
B: That's upper.
D: That's upper motor neuron, rather than thinning and weakening, which is lower.
B: Uh huh.
D: People who have primarily upper motor neuron dysfunction have generally a much better outlook. Generally a slower form of the disease. Generally do much better.
B: OK.
D: So the age and the predominance of the upper motor are very, very positive. And even though I hear you about your swallowing, everything that we see about your speech and swallowing muscles seem to be normal.
B: OK.
D: And everything that we see about your breathing muscles seems to be normal.
B: OK.
D: So when the, what we call the bulbar muscles, which are these muscles in here for speech and swallowing, the respiratory, the speech and swallowing muscles appear to us to be normal. These are two very positive prognostic factors. Both of those things. Either one of those being abnormal is serious. Both of them being normal, at the time of diagnosis, is very positive.
B: OK.
D: So, being a man is not quite as good as being a woman.
B: OK.
D: But it's not a big difference, but women actually seem to fair a little bit better than men. But that's a subtle difference. So you've got really most of the very positive prognostic factors going for you. And I have had people who have predominantly the upper motor neuron type, and who are predominantly young, who have normal breathing muscles and normal, apparent -- to us -- normal swallowing and speaking muscles, who have a very slow form of the disease. A much more benign type of ALS. I could be wrong. I love it when I'm wrong. But that's how it looks to me.
B: OK.
D: So having said the really serious, bad news that I do think this is ALS, I do want to say to you that it looks to me as though you may have a more slowly-progressive form than the great majority of people that we see.
B: Two questions.
D: Sure.
B: Um, first question is, how do I establish a metric and then sort of test and gauge myself in order to make a projection? And second thing is, what did you think of the brightness of the FLAIR signal in the MRI?
D: Well, the MRI is abnormal. And it does indicate to us that it's more confirming information. It does support the diagnosis of ALS. The pattern of that FLAIR signal is really very typical of ALS. And now that we're starting to become more experienced with the FLAIR images in MRI, we're finding that that can be very helpful in making a diagnosis or at least in supporting it.
B: OK.
D: It doesn't tell us anything good or bad, it just tends to say that it's really very typical of what we see in ALS.
B: OK. What about gauging, measuring my own progress?
D: Well, the things that are really important are of course your functionality, which you will be able to see very well. The things that we focus on are the breathing measurement, because generally speaking that is the most important single measurement that we make.
B: The 94, I scored a 94, is that cubic centimeters?
D: No.
Doctor2: It's a percentage of the average normal value.
B: OK.
D2: That's within the normal range.
B: It's a percentage.
D: It's percent of predicted.
B: Like the typical population at my age or whatever.
D2: Your height...
B: Would be 100 percent, sorry, would be 100. And I was 94.
D2: Right.
D: You're at the 94th percentile...
B: Percentile.
D: ...of people for your age...
B: Yes.
D: ...weight, height, and gender.
B: So when...
D: We have a huge data bank and when anyone is over the 85th percentile, of the huge data bank...
B: Yes.
D: Your familiar with the [Gestures]...
B: The bell-curve, yeah...
D: ...the bell-shaped curve, you're what we would consider normal.
B: OK.
D: So that measurement, as we're very experienced with it, and do that each time we see people with ALS, allows us to kind of track how things are going.
B: 94th percentile -- sorry to interrupt -- 94th percentile actually, to me seems very good. I mean, like, when I took--
D2: It's not exactly a percentile. It's a percentage. Of a predicted value.
B: OK.
D2: Which would be a 100 percent, and you're 94 percent.
B: All right. Sorry, I interrupted you.
D: So, are we OK then so far, with what we have?
B: Yeah, I just--
D: Most people do have a periodic visit to a center like this, where we make measurements, and kind of give feedback about how things are going. The average person comes here about every three months. This may or may not be appropriate for you, but we can tell you what our resources are and you can decide whether you want to use us any in the future. The big things that we do here are, first of all, we're heavily involved in research, and we're testing new compounds, and I'll tell you about that if you're interested.
B: The availability of studies, clinical trials?
D: Yes, yes, right. And then the second thing is that, um, we have a comprehensive team of experts in every conceivable aspect of this condition. Hand functions, speech functions, swallowing functions, nutrition, exercise, mobility, on and on. Every aspect of the disease is represented in our team of experts for rehabilitation and for giving therapies and things that would help you.
B: Yeah.
D: So what you might consider is coming here one time to see what the team could offer you in a one-stop shopping sort of thing, and that would probably be something that you would want to allow a half day for, and sometime in the next month or two, depending on your schedule. And you'd get a good feel for what we have available. And most people find it extremely helpful. So, we would -- and, and the average person comes here about every three months for that kind of comprehensive care and evaluation and indication of how things are going and what can be done.
B: Yeah.
D: So, and then, on the research side we're testing some new compounds that we think are very promising, very exciting. And we'd be happy to give you some information about that, for you to decide whether you might be interested.
B: Oh, yeah.
Wife: I think one concern that we discussed is, what's the chance, of our testing them, that he might wind up getting a placebo rather than the actual substance?
D: Right. So everybody has a chance of getting a placebo, and some people decide that if there's a chance of getting a placebo, they're really not interested, and we totally understand that because being in research is optional. Other people say: What do I have to lose? If I do nothing, I have no chance of benefiting myself or helping other people or really fighting to stamp out the disease. So, to some extent there is an altruistic motive, but to some extent there is a motive of possibly getting benefit. And then the third thing that happens with the people who are in the trials are first of all, there's a tremendous sense of optimism in people who are in trials compared to those who aren't, and people who are in trials come here regularly and actually get better care, because they not only have a finger on the pulse of what's happening, but they get a lot of attention when they're coming here. There's no cost for any of that, it's all, all free.
B: And typically you're only in one trial at a time?
D: Yes, you do have to kind of 'pays your money and takes your chances.'
B: You can go sequentially, right?
D: Well, you can do one and then do another.
B: OK.
W: So currently for the treatment of ALS or trying to slow the progression there's not like a cocktail of drugs the way there is for HIV?
D: That's where we're moving. We want to develop a cocktail. At the moment we have one drug, riluzole. And, you're not taking it, right?
B: No I am not.
D: So we'll discuss that next.
B: OK.
D: But where we're going is to get multiple drugs. We have this on drug that slows down the disease course. It's very safe. And what we want is to develop a cocktail of drugs like AIDS and leukemia. We do know that high doses of vitamin E, added on to the riluzole, add or enhance its effect a little bit. So we do recommend 2000 vitamin E a day with some lipid or fat or milk or something in the tummy to help facilitate the absorption of it.
B: [Fumbles for pen]
D: You've got it on tape.
B: Yeah! I got it on tape. Yeah.
D: [Laughing] You've go everything here, you don't have to write down a single thing!
B: No, I...
D: And where we're after is another drug or two to add to that cocktail. So we have the beginnings of a cocktail. So this drug riluzole suppresses too much glutamate, which appears to be an issue.
B: Glutamate.
D: The buildup of glutamate in motor areas in ALS that appears to cause some of the mischief. And riluzole blocks that, and it does slow down the disease process. And even though the literature on riluzole says it gives you an extra couple of months, that was on the results of people tested who were much farther along the disease course than you. And what we're now seeing, in Ireland and in Britain and in other registries where people are starting the drug earlier, that there's a substantial benefit from the drug. It's very safe, but it is very expensive. And so, um, you would have to decide about the cost factor because, Kaiser used to pay for it, and now my understanding is that they may not longer be covering the drug.
B: Just FYI, I'm on Blue Cross PPO.
D: [Thumbs-up sign].
B: Yeah. [Thumbs-up sign]
D: Good. Sounds good.
B: Um, but...
D: So do you have questions about the drug.
B: Um, tell me about the...
D: It's a pill.
B: ...the cost factor.
D: You take it twice a day. Well, if you're just buying it, it's 800 a month.
B: Flat. Eight hundred a month?
D: Something like that, you know, give or take--
B: But then I have some, I do have coverage, so they'll pick up the, hopefully part of it. But I just want to respond and says, yes, you guys are the experts and I do want to avail myself and be involved here and probably be in some of the clinical trials...
D: Great.
B: Um, riluzole sounds very interesting. I was supposed to ask you about that. Um, there are -- you mentioned the vitamin E. There are various question that I have. You probably have literature that can answer them, so I really don't need to take up your time about what should I do now, right? Um, do you think it is a bad idea -- I'm taking 2.1 grams of creatine, uh, have been since the 18th of January. Is that a bad idea?
D: No.
B: OK.
D: For now I wouldn't change that.
B: OK.
D: Uh, and for now I would only do two new things.
B: OK.
D: Add 2000 of vitamin E, and then, riluzole.
B: OK.
D: And not try, not do multiple things at the same time.
B: Right.
D: So, and then, when you get stabilized on those, on the vitamin E and riluzole, and the creatine, then we can talk about whether other things might be useful.
B: OK. Can I get a prescription for riluzole? [points to second doctor]. You're -- That's what you're. [Laughs] OK. And can I fill it somewhere around here?
D: Well, here's the deal...
B: Or, or the...
D: Yes, and yes. But just be aware that for you to get riluzole from the Kaiser system, that would have to be prescribed by a Kaiser neurologist.
B: I'm on the PPO. Blue Cross, not Kaiser.
D: OK.
B: Um. Can you briefly, very briefly, tell me what, now what is creatine?
D: Well creatine is a supplement that actually has a beneficial impact on the mitochondria. The mitochondria is the energy factory of the cells.
B: Right.
D: So the good news is that in a mouse model of ALS, creatine prolongs survival and seems to really be of substantial benefit. The bad news is that two studies that have been done so far in patients with ALS, using creatine, have so far shown no benefit.
B: Right.
D: There is a third study under way though, looking at it in a new way [gestures], and so, that's what it does.
B: OK. Is it ... It is not a hormone, right?
D: No.
B: DHEA if I understand it is a...
D: That's a hormone.
B: ...hormone precursor? Or is it a hormone?
D: Well, it's a hormone and it's a hormone precursor.
B: OK.
B: Creatine is just ... what ... is it an enzyme or a protein? I don't know?
D: Um, I don't know how to classify it.
B: OK.
D: [To second doctor] Do you know how to classify it?
D2: It's a protein.
W: Amino acid?
B: Apparently they've known about it since, like 1859.
D: Oh, yeah.
B: OK. [To wife, running camera] You have a list of questions.
W: Well, already some of them have been answered, but I did want to ask about the role of exercise. I mean, [B] has been trying to run or lift weights and do yoga, whatever. He's done something almost every day, sort of on the theory of you either lose it, uh, use it or lose it. And so, I'm wondering if that's something... Maybe it's something a physical therapist would address more.
D: Well, if you come to our clinic, our physical therapist will address that in great detail. But what I would say to you is that uh, we are bullish about exercise. And we feel that it's helpful, and desirable. The only caveat there is, we don't like to see people overdo. So, when you feel tired, stop.
B: OK.
D: And if you have pain the next day, you overdid. And, short of that, no problem.
B: OK.
W: OK, well, then I wondered about other factors, and would they have any effect on the, diagnosis. For instance like having a high cholesterol, does that have anything to do--
D: No.
W: Would it effect the disease at all?
D: No.
W: OK. Let's see. I was happy to hear that he falls into the category of having a slower rate, or...
D: Yeah.
W: There are several factors that point towards that.
D: We interpret that as being very positive.
W: Um.
B: That is very positive, yeah.
W: Yeah, and we have two, because we have two small children, and the thing that came to my mind when we first heard the diagnosis was that, you know, if he was you know, needing to breathe with a respirator any time soon, we're going to be bringing home all kinds of germs from school, and how do you handle that?
D: OK. If and when we come to that, which is way down the road, don't worry, we'll all deal with that.
W: OK, and then ah, yeah I guess you've answered most of these, most of my questions. I guess the last thing was that I looked at one website that suggested that as soon as you've gotten the diagnosis, the whole family should go into counseling, but with a four-year-old and a one-year-old, it doesn't seem the right thing to do, so what would you recommend?
D: Well first of all, when we say the whole family, we're really talking about the two of you. Uh, little kiddos, uh, you know, wouldn't really be able to comprehend this and we don't recommend making any big deal out of it for little kids. You know, if they were a little older, or if you were having more trouble, they would need to have some explanation, but it should be something very simple. 'Dad's having trouble with his leg, it's nothing to worry about.'
B: Yeah. Right.
D: That type of thing. For older kids it's a different story, but for little kids that's what we recommend.
B: Yeah, I thought so.
D: So, the other things that we know that a correlated with longevity with this disease...
B: Yes.
D: ...are not giving up, or giving in, having an upbeat attitude, having a strong support system, and ...
D2: We're three for three.
B: Yeah! [Laughter].
D: And the other one is, uh, not getting depressed. Or, if one does get depressed, having some treatment for depression. Many people get depressed with this condition, and often it's temporary. Have you been depressed since this has come up?
B: No, I've been, at times, we've been angry or just very distraught.
D: Yes.
B: But that usually lasts -- I feel a little that way now, just thinking about it.
D: Yes.
B: But that lasts a couple of hours. But I'm really a very positive person.
D: Yes.
B: I'm not trying to, I don't force. When I was a boy, between like ages 9 and 19, OK, I was depressed. So I know what that feels like. I'm not depressed. And I ...I don't. I don't think I'm at risk but I'll watch out for it.
D: So, do that. Only in the sense that, hey, we can give you medications for that that would really be helpful.
B: Sure.
D: [To wife] And you too need to look for that in yourself.
W: Uh huh.
D: As well as in him. Because we use antidepressants here like water. And often we need them only for a short time. And many people do need them. And it just speeds the adjustment tremendously for people who do get down.
B: OK.
D: So just keep an eye peeled. It doesn't happen to everybody. But if it does happen, just be aware and support each other and know that treatment really makes a lot of sense, with some medication.
B: I know you have tremendous resources here. How do I get on that train? Like, I could go home and get in ... get distracted and... What I'm saying is, how do I involved?
D: Plugged in?
B Plugged in. Sorry, that's--
D: Well we have two team members who are here who can plug you in. They're going to come in and talk to you.
B: Good. Excellent.
D: You OK, for the time?
B: Yeah. That's perfect.
D: OK.
B: Yeah.
D: Any other questions right now?
W: I was just wondering, are there alt-- I mean, you said the riluzole is the drug that's most, got the most, ah, experience behind it and so then that's what you recommend to start with. Is there--
D: It's the only FDA-approved drug...
W: I see.
D: ...to slow down the disease. And then vitamin E we say because it seems to enhance the riluzole effect.
W: So, as far as starting on something that would perhaps have a positive effect, that would be the only alternative right now at this point.
D: Right. And then if one decides about the clinical trails, to participate in a trial, that has the real potential of helping too.
B: Yeah, I'm excited about that.
D: Good.
B: I have two questions for you. One may make you laugh, ridiculous. I used to be a knuckle cracker. All the time. And I forced myself to stop cracking my knuckles probably, maybe seven years ago. Any even remote possibility that this --
D: No.
B: OK. Next question.
D: Let me just say, everybody wants to know what brought this on. Everybody.
B: And we don't know that the cause is.
D: You got it.
B: Yeah.
D: You got it.
B: OK.
D: It's nothing you did wrong.
B: All right.
D: For sure. It's nothing you did wrong.
B: OK. Next, and this is the harder question: Can you, please -- and I know this is difficult. Can you give me the rosy scenario in terms of number of years and how functional, and when I might eventually die of this, and give me the dark scenario.
D: Well the dark is that you could die within a year. Highly unlikely, given the things that I've already told you about. The rosy scenario ... the rosiest scenario...
B: Yeah.
D: ...is that this might turn around and even go away. I've seen that.
B: How often -- how -- what percentage of people does that happen to?
D: Small.
B: Very small.
D: Yes.
B: OK. Let's assume it doesn't go away.
D: Then the next most rosy scenario is that this goes very slowly, and a year from now we're sitting looking at each other and the differences are very modest.
B: OK.
D: Little more trouble with the hand, little more trouble with the leg. A year later we're getting together, and it's still only in the left arm and leg and we're still looking at a only a little bit of worsening. And I have seen that.
B: OK.
D: So, that's -- worsening over time -- but very, very slowly. So that would be second-best rosy scenario.
B: Gimme a number on that one.
W: Percentage.
B: I know it's hard.
D: What percent?
B: No, when do I die, basically, under the, the sec--
D: Well, the first one, obviously you would not have shortened life.
B: Right. Right.
D: Complete recovery.
B: The second...
D: The second one, you might have a normal life span.
B: OK. That's what I intend.
D: Yes. Absolutely. And you know the one patient that I can think of very clearly who did fully recover from this is now 96 years old.
B: Wow.
W: Wow.
D: Absolutely full of spit and vinegar and refused...
B: Yeah.
D: ...to let this get her down.
B: Yeah.
D: And, I swear, it was the attitude.
W: How old was she when she was diagnosed?
D: 72.
W: Yeah.
D: I've been seeing her for 24 years.
B: Amazing.
B: Can I ask you both a question?
D: And then I have to go.
B: OK. Um, my right side, um ... how impaired does it seem? I mean, I notice, I can do this [tapping forefinger on thumb rapidly] but I my wife, and you, can do it faster.
D2: Yeah.
D: And so I would say, minimal.
B: OK.
D: Minimal.
B: All right. All right. Well, I thank you. [Handshake].
D: So we're going to have a couple of other people come in and talk with you about what services we have, and the clinic, and so forth.
B: OK.
D: And then, um, we're here for you.
B: All right.
D: So whatever you decide... I know you're going to be checking back in with Dr. XXXXXXXXX. Many people use our services along with their local neurologist, and find that there's different benefits for both. Some people just go back to their neurologist. That's fine. Other people just come here. And any admixture, whatever works for you, we will work with.
B: OK. All right.
W: What would you say that the local neurologist could offer that you could not, or that he could offer more easily?
D: Proximity.
W: Yeah.
B: Like, 'Hey, look at this!'
D: You got it.
B: OK.
W: Thank you.
D: Thanks.
D2: I have a few things for you.
B: OK.
D2: [To camera] And... Cut!
W: OK.
[next tape segment]
B: Big Whoop!